January 1 is the hallmark of new beginnings—and for physicians and hospital clinics, this year will be no different. January 1, 2019 marks the first opportunity for eligible physicians and hospital clinics to earn penalties and incentives for performance through one of Medicare’s Quality Payment Programs, the Merit Incentive-Based Payment System (MIPS).
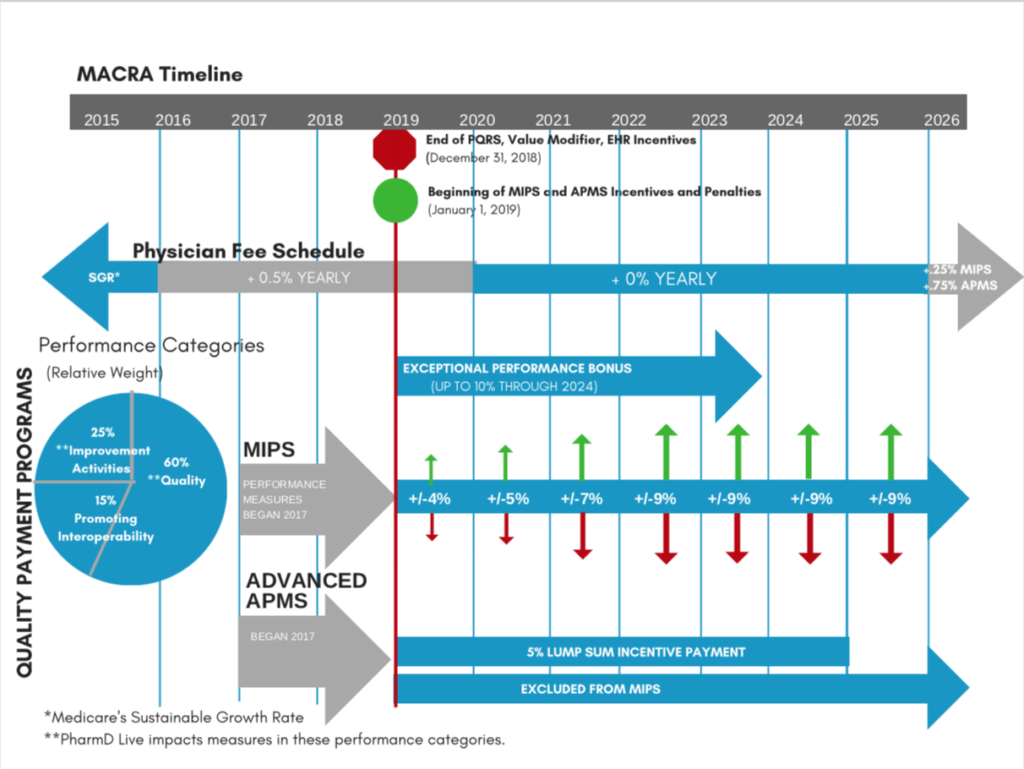
MIPS replaces the PQRS (Physician Quality Reporting System), the Value-Based Payment Modifier and the Electronic Health Record (EHR) incentive program. Borne from the Medicare and CHIP Reauthorization Act (MACRA) of 2015, MIPS and APM (Alternative Payment Models) are the two available options for quality payment tracks. MIPS is the default track, and its performance categories include Quality (60%), Improvement Activities (25%) and Promoting Interoperability (15%).
In theory, value-based care makes perfect sense. Catalyzing the best outcome at the lowest cost seems straightforward and reasonable by any measure. The Centers for Medicaid and Medicare Services (CMS) couches it as a four-step process: “Collect data, Report data, Feedback available, Payment adjustment.”
Butmoving from theory to practice has presented challenges, sowing frustration in physicians driven by patient care. Physicians and practice administrators envision stacks of paperwork, a quagmire of regulations and processes ad nauseum.
And studies reveal physician’s fears and perceptions are based in reality. Research by Weill Cornell Medical College and the Medical Group Management Association (MGMA) in 2016 showed physicians spent 15.1 hours every week processing quality metrics. Time spent on the intricacies of reporting, tracking metrics and understanding accompanying regulations cuts into patient care.
Success in the value-based framework requires deft planning and patience—which demands the scarcest resource for many physicians: time. As you know, value-based care is not an ephemeral trend; rather, a way of providing care that will catalyze a seismic change in its provision.
To begin planning for 2019:
Review the timeline of implementation.
- Review quality measures and compare against current top-performing practice areas.
- Review your business model. Get acquainted with new reimbursement codes which enable telehealth.
- Choose a third party telehealth chronic care management provider, such as PharmD Live, adept in streamlining billing reports and quality measures data and providing care coordination and management.
Many physicians and hospital clinics have chosen to partner with a third party care management team, such as PharmD Live, as an element of their MACRA strategy. PharmD Live serves as a seamless extension of your practice, providing turnkey, pharmacist-led chronic care management services to boost quality metrics, increase revenue and streamline care. To learn more about PharmD Live’s pharmacist-led care, schedule a consultation.
This article is the first in a series dedicated to helping physicians and hospital clinics prepare for MIPS in 2019.








